Overview

Flatfoot (pes planus) is a condition that occurs when the arch or instep of the foot collapses or touches the standing surface. It is also known as fallen arches or pronation of the feet. The human foot is made up of 26 bones, 33 joints, and over 100 muscles, tendons and ligaments. The arch of the foot is created by tightening of the muscles and various ligaments that support the bones of the arch as well as ligaments that run from the heel to the ball of the foot. The arches distribute weight evenly across the feet and up the legs, and can affect walking. A well-developed arch is balanced between rigidity (for stability) and flexibility (for adapting to surfaces).
Causes
Fallen arches in adults are caused by several things. Below are some of the most common causes. Abnormalities present from birth. Torn or stretched tendons (resulting from foot injuries or foot strains). Inflammation or damage of the PTT (posterior tibial tendon). The PTT is responsible for connecting the middle of the arch to the ankle and lower leg. Dislocated or broken bones (also as a result of injury). Health problems like rheumatoid arthritis. Nerve problems. Other factors like diabetes, obesity, aging and pregnancy (these factors are known to increase the risk of fallen arches).
Symptoms
Symptoms that should be checked by a pediatrician include foot pain, sores or pressure areas on the inner side of the foot, a stiff foot, limited side-to-side foot motion, or limited up-and-down ankle motion. For further treatment you should see a pediatric orthopedic surgeon or podiatrist experienced in childhood foot conditions.
Diagnosis
Determining whether you have fallen arches may be as easy as looking at the shape of the middle bottom of your foot. Is there any kind of arch there? If you cannot find any kind of arch, you may have a flat foot. There are, however, other ways to decide in case you're still not sure. Another way to figure out if you have flat feet is to look at a few pairs of your shoes. Where do you see the most wear on the heels? If you notice significant wear in the heel and the ball of the foot extending to the big toe, this means you are overpronating. Overpronators roll their feet too far inward and commonly have fallen arches. To figure out if you have flat feet, you can also do an easy test. Get the bottoms of your feet wet and then step on to a piece of paper carefully. Step off the paper and take a look at the print your foot made. If your print looks like the entire bottom of a foot, your feet are flat. People with an arch will be missing part of the foot on their print since the arch is elevated off of the paper. Regular visits to your podiatrist are highly recommended.
arch support inserts reviews
Non Surgical Treatment
Treatment isn't usually needed for flat feet because the condition doesn't usually cause any significant problems. Aching feet can often be relieved by wearing supportive shoes that fit properly. You may need to wear shoes that are wider than normal. If your feet overpronate, you may need to wear a special insole (an orthotic) inside your shoes to stop your feet rolling inwards when you walk or run. These will usually need to be made and fitted by a podiatrist. Stretching your calf and Achilles tendon may also help as a tight Achilles can make your foot overpronate. To stretch your calf and Achilles tendon, step forwards with your left leg and bend it, with your right leg straight and both feet pointing forwards, push your right heel into the ground while keeping your right leg straight; you should feel the stretch at the back of your right leg, below the knee, hold the stretch for 15 to 30 seconds and repeat with the opposite leg, repeat the stretch two to four times on each leg, and repeat the overall exercise three to four times a day.
Surgical Treatment

Surgery for flat feet is separated into three kinds: soft tissue procedures, bone cuts, and bone fusions. Depending on the severity of the flat foot, a person?s age, and whether or not the foot is stiff determines just how the foot can be fixed. In most cases a combination of procedures are performed. With flexible flat feet, surgery is geared at maintaining the motion of the foot and recreating the arch. Commonly this may involve tendon repairs along the inside of the foot to reinforce the main tendon that lifts the arch. When the bone collapse is significant, bone procedures are included to physically rebuild the arch, and realign the heel. The presence of bunions with flat feet is often contributing to the collapse and in most situations requires correction. With rigid flat feet, surgery is focused on restoring the shape of the foot through procedures that eliminate motion. In this case, motion does not exist pre-operatively, so realigning the foot is of utmost importance. The exception, are rigid flat feet due to tarsal coalition (fused segment of bone) in the back of the foot where freeing the blockage can restore function.

Flatfoot (pes planus) is a condition that occurs when the arch or instep of the foot collapses or touches the standing surface. It is also known as fallen arches or pronation of the feet. The human foot is made up of 26 bones, 33 joints, and over 100 muscles, tendons and ligaments. The arch of the foot is created by tightening of the muscles and various ligaments that support the bones of the arch as well as ligaments that run from the heel to the ball of the foot. The arches distribute weight evenly across the feet and up the legs, and can affect walking. A well-developed arch is balanced between rigidity (for stability) and flexibility (for adapting to surfaces).
Causes
Fallen arches in adults are caused by several things. Below are some of the most common causes. Abnormalities present from birth. Torn or stretched tendons (resulting from foot injuries or foot strains). Inflammation or damage of the PTT (posterior tibial tendon). The PTT is responsible for connecting the middle of the arch to the ankle and lower leg. Dislocated or broken bones (also as a result of injury). Health problems like rheumatoid arthritis. Nerve problems. Other factors like diabetes, obesity, aging and pregnancy (these factors are known to increase the risk of fallen arches).
Symptoms
Symptoms that should be checked by a pediatrician include foot pain, sores or pressure areas on the inner side of the foot, a stiff foot, limited side-to-side foot motion, or limited up-and-down ankle motion. For further treatment you should see a pediatric orthopedic surgeon or podiatrist experienced in childhood foot conditions.
Diagnosis
Determining whether you have fallen arches may be as easy as looking at the shape of the middle bottom of your foot. Is there any kind of arch there? If you cannot find any kind of arch, you may have a flat foot. There are, however, other ways to decide in case you're still not sure. Another way to figure out if you have flat feet is to look at a few pairs of your shoes. Where do you see the most wear on the heels? If you notice significant wear in the heel and the ball of the foot extending to the big toe, this means you are overpronating. Overpronators roll their feet too far inward and commonly have fallen arches. To figure out if you have flat feet, you can also do an easy test. Get the bottoms of your feet wet and then step on to a piece of paper carefully. Step off the paper and take a look at the print your foot made. If your print looks like the entire bottom of a foot, your feet are flat. People with an arch will be missing part of the foot on their print since the arch is elevated off of the paper. Regular visits to your podiatrist are highly recommended.
arch support inserts reviews
Non Surgical Treatment
Treatment isn't usually needed for flat feet because the condition doesn't usually cause any significant problems. Aching feet can often be relieved by wearing supportive shoes that fit properly. You may need to wear shoes that are wider than normal. If your feet overpronate, you may need to wear a special insole (an orthotic) inside your shoes to stop your feet rolling inwards when you walk or run. These will usually need to be made and fitted by a podiatrist. Stretching your calf and Achilles tendon may also help as a tight Achilles can make your foot overpronate. To stretch your calf and Achilles tendon, step forwards with your left leg and bend it, with your right leg straight and both feet pointing forwards, push your right heel into the ground while keeping your right leg straight; you should feel the stretch at the back of your right leg, below the knee, hold the stretch for 15 to 30 seconds and repeat with the opposite leg, repeat the stretch two to four times on each leg, and repeat the overall exercise three to four times a day.
Surgical Treatment

Surgery for flat feet is separated into three kinds: soft tissue procedures, bone cuts, and bone fusions. Depending on the severity of the flat foot, a person?s age, and whether or not the foot is stiff determines just how the foot can be fixed. In most cases a combination of procedures are performed. With flexible flat feet, surgery is geared at maintaining the motion of the foot and recreating the arch. Commonly this may involve tendon repairs along the inside of the foot to reinforce the main tendon that lifts the arch. When the bone collapse is significant, bone procedures are included to physically rebuild the arch, and realign the heel. The presence of bunions with flat feet is often contributing to the collapse and in most situations requires correction. With rigid flat feet, surgery is focused on restoring the shape of the foot through procedures that eliminate motion. In this case, motion does not exist pre-operatively, so realigning the foot is of utmost importance. The exception, are rigid flat feet due to tarsal coalition (fused segment of bone) in the back of the foot where freeing the blockage can restore function.




 Morton's neuroma is an inflammation of the nerves in the foot that go to the toes. Although the name includes the word ?neuroma,? it is not really a tumor. It can affect any of the toes in the foot. However, it most often affects the nerves that run between the third and fourth, or second and third toes.
Morton's neuroma is an inflammation of the nerves in the foot that go to the toes. Although the name includes the word ?neuroma,? it is not really a tumor. It can affect any of the toes in the foot. However, it most often affects the nerves that run between the third and fourth, or second and third toes.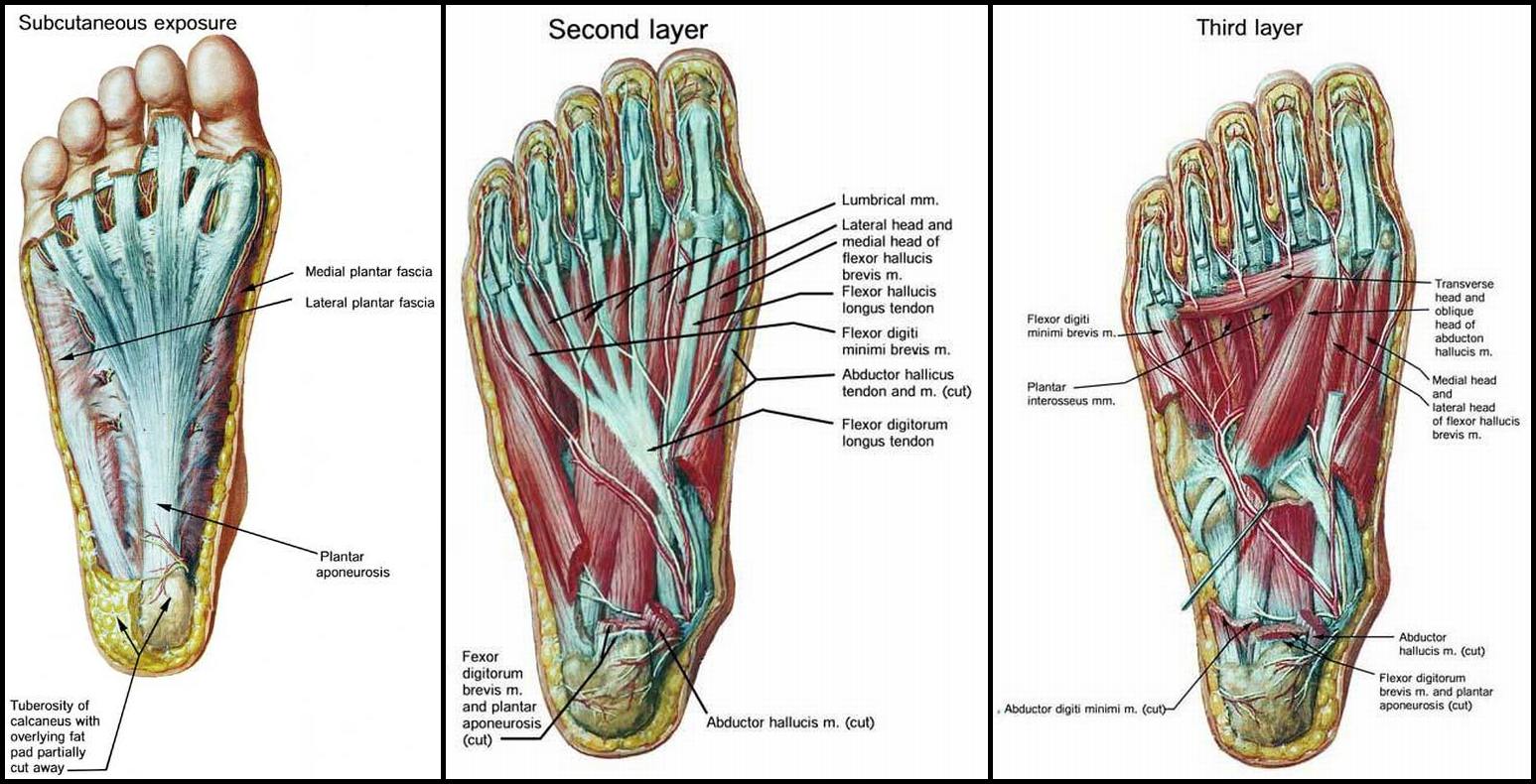



 Overview
Overview Symptoms
Symptoms Prevention
Prevention Your first toe or ?big? toe is medically referred to as the hallux, and is the hardest working toe of your foot because it pushes you off the ground as you walk and run. More than 50% of Women in the UK have bunions, therefore is a common deformity. The problem often runs in families although tight narrow shoes and high heels are often blamed. We offer bunion surgery to help with this problem.
Your first toe or ?big? toe is medically referred to as the hallux, and is the hardest working toe of your foot because it pushes you off the ground as you walk and run. More than 50% of Women in the UK have bunions, therefore is a common deformity. The problem often runs in families although tight narrow shoes and high heels are often blamed. We offer bunion surgery to help with this problem.


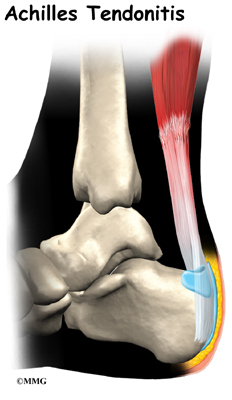 An Achilles tendon rupture is when you tear the tissue that connects your calf muscle to your heel bone. Your Achilles tendon is very strong and flexible. It?s at the back of your ankle and connects your calf muscle to the bone in the heel of your foot (calcaneum). If you rupture your Achilles tendon, you can either partially or completely tear the tendon. Most people who injure their Achilles tendon are between 30 and 50 and don?t exercise regularly. It?s more common in men but can affect anyone. It happens most often in the left leg. This may be because most people are right-handed which means that they ?push off? more frequently with the left foot when running.
An Achilles tendon rupture is when you tear the tissue that connects your calf muscle to your heel bone. Your Achilles tendon is very strong and flexible. It?s at the back of your ankle and connects your calf muscle to the bone in the heel of your foot (calcaneum). If you rupture your Achilles tendon, you can either partially or completely tear the tendon. Most people who injure their Achilles tendon are between 30 and 50 and don?t exercise regularly. It?s more common in men but can affect anyone. It happens most often in the left leg. This may be because most people are right-handed which means that they ?push off? more frequently with the left foot when running.
